Denial Management: Recover Revenue and Eliminate Guesswork
At Billopt, we know denials aren’t just a nuisance—they’re a hemorrhage of your hard-earned revenue. With 1 in 5 claims initially denied and 65% of those denials never reworked, practices lose thousands monthly to coding errors, payer loopholes, and administrative oversights. Our denial management service isn’t just about fixing mistakes—it’s about attacking the root cause, reclaiming every dollar, and future-proofing your revenue cycle.
Why Denial Management Can’t Wait
The average practice loses $50,000+ annually to unresolved denials. But the real cost? Wasted staff hours, strained cash flow, and lost trust in your financial processes. Payers are getting stricter, denial rates are rising, and manual follow-ups can’t keep up.
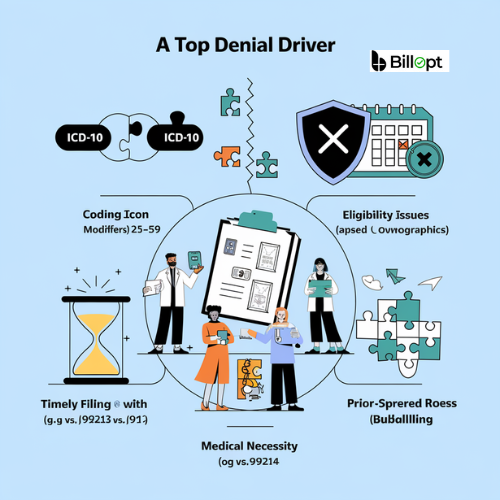
Top Denial Drivers We Fix:
-
Coding Errors (e.g., invalid ICD-10, missing modifiers like -25 or -59)
-
Eligibility Issues (lapsed coverage, incorrect patient demographics)
-
Timely Filing (missed submission deadlines)
-
Medical Necessity (missing documentation, mismatched CPT codes)
-
Payer-Specific Rules (unbundling, prior authorization gaps)
With Billopt, you don’t just react to denials—you prevent them.
How Billopt Transforms Denials into Dollars
1. Denial Triage & Analysis
-
AI-Powered Denial Tracking: Our system categorizes denials in real time by type, payer, and provider, spotting trends (e.g., "UnitedHealthcare denies 30% of modifier -59 claims").
-
Root Cause Audits: Certified coders dissect each denial to identify systemic issues (e.g., EHR setup flaws, staff training gaps).
2. Precision Appeals & Resubmission
-
Bulletproof Appeal Letters: Our AAPC-certified team crafts appeals using clinical evidence, payer policies, and regulatory guidelines (e.g., citing NCD/LCD rules for Medicare).
-
Peer-to-Payer Negotiation: Former insurance executives on our team escalate stubborn denials directly to payer medical directors.
-
Time-Sensitive Fixes: Resubmit corrected claims within 48 hours to avoid timely filing rejections.
3. Proactive Denial Prevention
-
Coding Guardrails: Real-time alerts flag high-risk claims (e.g., telehealth codes without GT modifier) before submission.
-
Staff Education: Monthly reports highlight recurring denial triggers, paired with targeted training for your team.
-
Payer Policy Updates: Automatic rule adjustments in your EHR as payers change requirements (e.g., new prior auth rules for MRI scans).
4. Recovery & Reconciliation
-
Denial Recovery Dashboard: Track recovered dollars, open appeals, and denial trends in real time.
-
Post-Recovery Audits: Ensure corrected payments match EOBs and contracts (e.g., catching underpayments on tiered fee schedules).
What Makes Billopt’s Denial Management Unmatched
Certified Denial Specialists
-
CPB (Certified Professional Billers): Experts in payer policies and appeals.
-
CPC (Certified Professional Coders): Masters of ICD-10, CPT, and HCPCS coding nuances.
-
CRCR (Certified Revenue Cycle Representatives): Trained in compliance and A/R best practices.
Technology That Outsmarts Payers
-
Denial Predictive Analytics: AI forecasts denial risks based on historical data (e.g., "Aetna denies 25% of your 99214 codes—let’s fix documentation").
-
Automated Workflows: Auto-assign denials to specialists by type (e.g., coding vs. eligibility).
-
Payer Rule Database: 10,000+ payer-specific guidelines loaded into our system (e.g., Cigna’s modifier -76 rules).
Specialty-Specific Strategies
-
Surgical Specialties: Tackle denials for procedures like arthroscopy (29827) or spinal fusions (22612).
-
Primary Care: Fix E/M coding denials (99213 vs. 99214) and chronic care management (99490).
-
Mental Health: Resolve telehealth (90837) and time-based coding disputes.
-
Diagnostics: Fight radiology (72148) and lab denials with medical necessity proof.
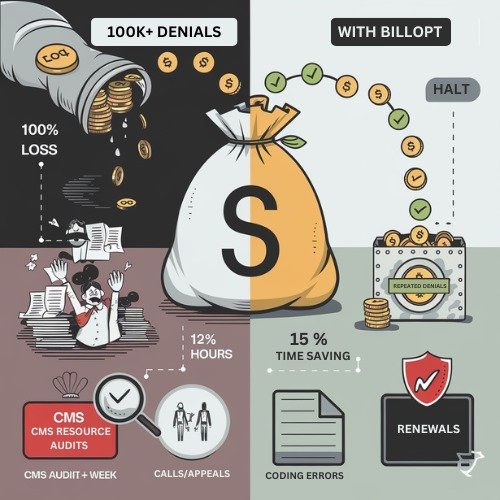
The Cost of Ignoring Denials
-
Revenue Leakage: 15% of denials are never appealed, costing practices $100k+/year.
-
Staff Burnout: 12+ hours/week wasted on manual appeals and phone calls.
-
Compliance Risks: Unresolved denials trigger audits (e.g., repeated coding errors flag CMS scrutiny).
Billopt’s Fix
-
90% Denial Recovery Rate
-
50% Reduction in Denial Volume within 6 months
-
100% Audit-Ready Documentation
Why Practices Trust Billopt





Ready to Stop Denials from Draining Your Revenue?
Don’t let payer loopholes and coding errors sabotage your bottom line. Billopt’s denial management service turns your A/R department into a revenue-recovery powerhouse.
Claim Your Free Denial Audit Today!
